What is Long QT syndrome?
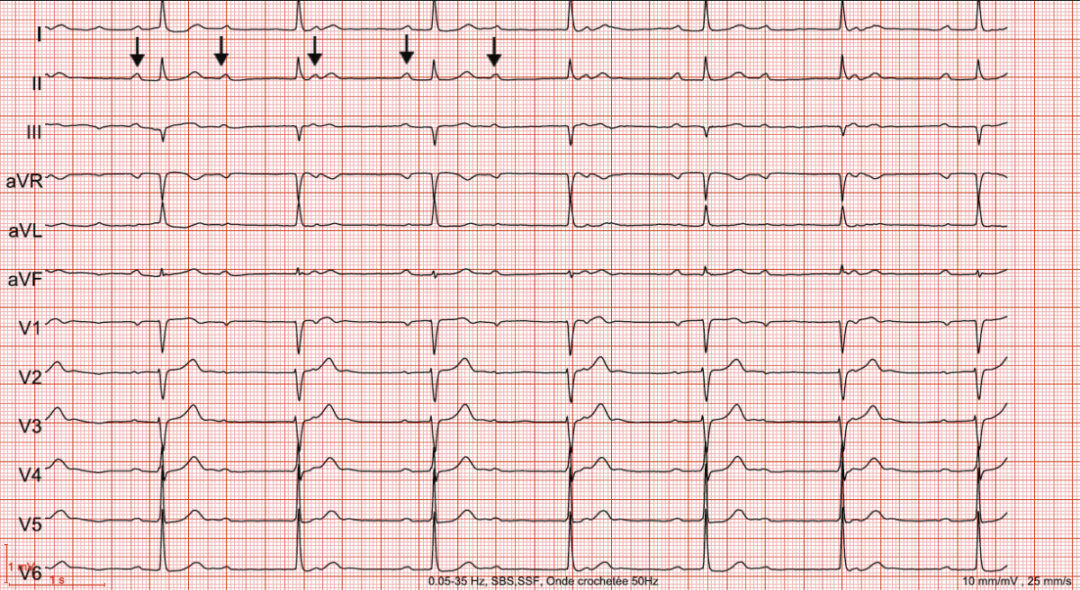
The “QT” or “QT interval/segment” is a portion of the electrocardiographic wave that reflects cardiac repolarization. The electrocardiogram (ECG), a routine examination in electrophysiology, records the heart’s electrical activity in the form of an electrocardiographic wave.
This wave appears as a series of repetitive complexes corresponding to the activation of the heart with each beat. These complexes, called “P-QRS-T complexes,” can be broken down into several segments or waves, each with its own meaning:
- The P wave: corresponds to the electrical activation (depolarization) of the atria;
- The PQ interval: corresponds to the electrical conduction between the atria and ventricles;
- The QRS complex: corresponds to the electrical activation (depolarization) of the ventricles;
- The T wave and QT interval: correspond to the electrical relaxation (repolarization) of the ventricles.
Most heart conditions can be associated with an abnormality in one of these waves, which makes the electrocardiogram particularly useful for the electrophysiologist in establishing a diagnosis.
Long QT syndrome refers to the finding on an electrocardiogram of a QT interval measurement that is longer than it should be. This reflects a prolongation of the duration of cardiac repolarization beyond normal values.